CUHK
News Centre
CUHK’s New Prostatic Artery Embolization Shows 90% Success Rate in Relieving Symptoms of Benign Prostatic Hyperplasia
The Department of Imaging and Interventional Radiology at The Chinese University of Hong Kong (CUHK) has initiated a clinical study on prostatic artery embolization (PAE) since 2014 and put the new treatment into clinical trial on benign prostatic hyperplasia (BPH) beginning in June 2015. The preliminary result is encouraging. 90% of the patients could pass urine in 2 weeks after the treatment. The team will continue the clinical study to collect further data with the aim of providing a non-surgical treatment option for the patients in the future.
【Benign Prostatic Hyperplasia (BPH)】
The prostate is a male sex gland which produces a thick fluid that forms part of the semen. BPH is the non-malignant enlargement of the prostate gland. It is common among elderly men and the prevalence increases with age. When sufficiently large, the hyperplastic nodules compress the urethral canal to cause an obstruction of the urethra and interfere with the normal flow of urine. According to the Department of Health of the Hong Kong Government, BPH affects more than half of men aged over 60 years, and up to 90% of men aged over 80 years. As such, it is estimated that BPH occurs in over 400,000 men, based on the Mid-year Population for 2015 figures.
Although 50-60% of these patients do not have any clinical symptoms, BPH is a progressive disease that may give rise to symptoms of urinary urgency, urinary hesitancy, frequent urination, weak urine flow, urinary retention and even bloody urine. Incomplete voiding may increase the risk of urinary tract infection and urinary bladder stone formation. Other clinical consequences include acute urinary retention, chronic urinary retention and renal failure.
【Treatment for BPH】
In general, BPH patients with mild symptoms that do not cause significant disturbance to daily lives can be treated conservatively, whereby patients are monitored with regular medical examinations. Doctors will consider medical treatment depending on the size of prostate gland and the symptoms. Patients who cannot pass urine would require Foley catheterization and subsequently surgery such as transurethral resection of the prostate (TURP).
Prof. Anthony Chi Fai NG, Director, S.H. HO Urology Centre, Department of Surgery, CUHK, remarked, ‘If medical treatment does not reduce a patient’s urinary symptoms, TURP may be considered to resect prostatic tissue through transurethral cystoscopy. TURP is currently the most effective treatment for BPH. However, 80% of patients may have complications of sexual dysfunction problems such as retrograde ejaculation and erectile dysfunction after the procedure.’
【Prostatic Artery Embolization (PAE)】
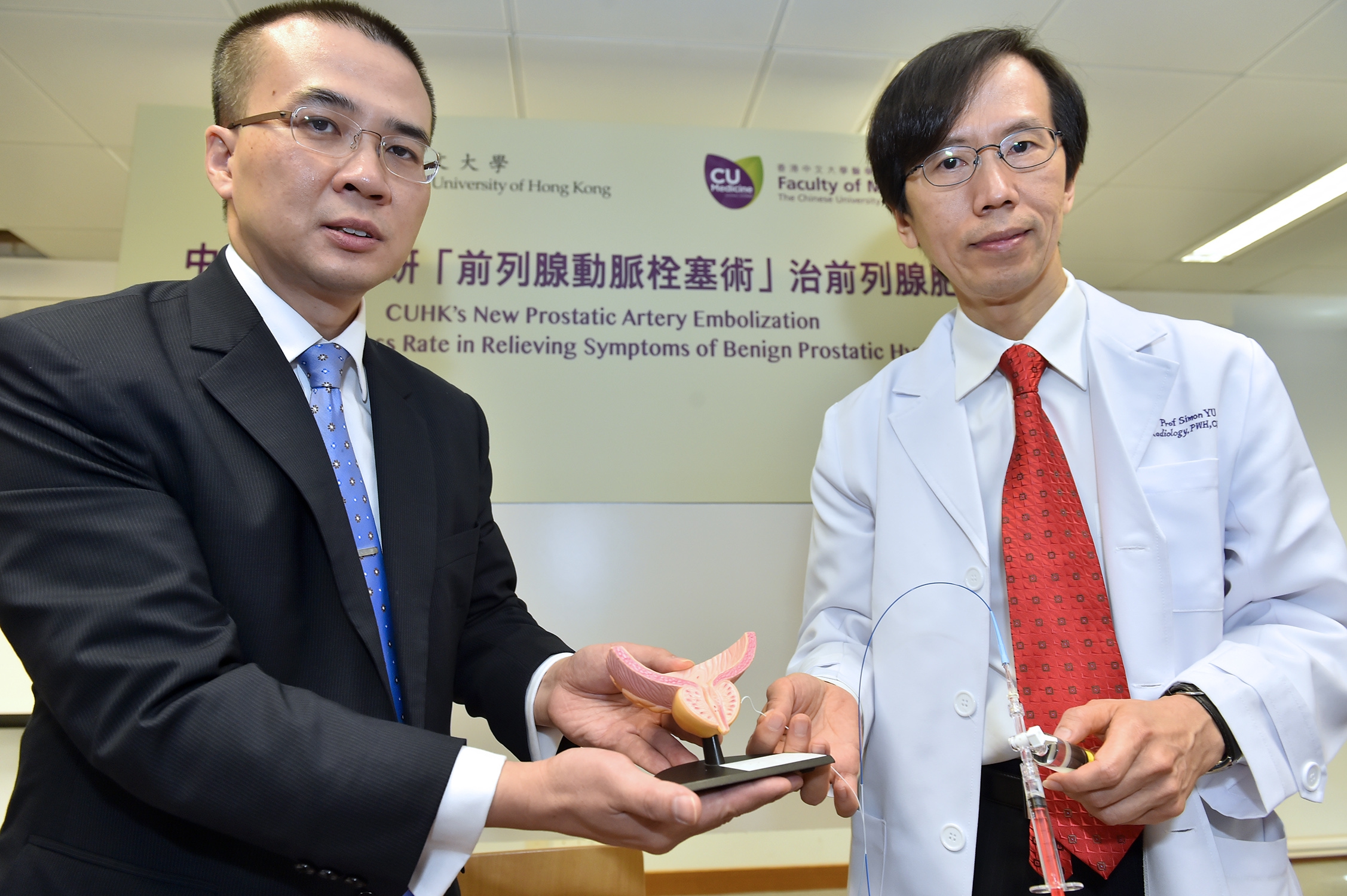
Since 2014, the Department of Imaging and Interventional Radiology at CUHK has initiated the clinical study on PAE, which involves the embolization of the prostatic arteries using microspheres of 100 to 300 micron in diameter through superselective catheterization of the arteries under X-ray control. Embolization leads to ischemic necrosis and volume reduction of the prostate. As a result, obstruction to urine outflow from the urinary bladder is relieved.
Ten patients have been treated since June 2015 without complication, with 9 of them passing urine in 2 weeks after PAE treatment. Prostate volume reduction was detected on magnetic resonance imaging (MRI) in 2 weeks. Urine flow rate progressively increased over 2 weeks and symptoms of BPH were reduced correspondingly.
Prof. Simon Chun Ho YU, Chairman, Department of Imaging and Interventional Radiology, and Director, Vascular and Interventional Radiology Foundation Clinical Science Center at CUHK, concluded, ‘Seven out of the 10 patients undergoing PAE had severe BPH to a degree of complete urinary retention, and required Foley catheterization of their urinary bladder before the treatment, indicating severe obstruction of their urethra. Six of them could pass urine 2 weeks after the treatment. Three other patients without Foley catheterization had improvement in urinary symptoms after the treatment. These preliminary results reveal that PAE is probably a safe and potentially promising minimally-invasive treatment for BPH.’
Professor YU went on to add that the treatment involves the use of catheters introduced through femoral vessels to the minute prostatic arteries and that PAE would not be feasible if there is severe atherosclerotic disease that preclude the access to the prostate arteries. The research team plans to recruit 40 subjects for study. BPH patients who are completely unable to pass urine and interested in participating in the study may call 2632 2046 for enquiries.
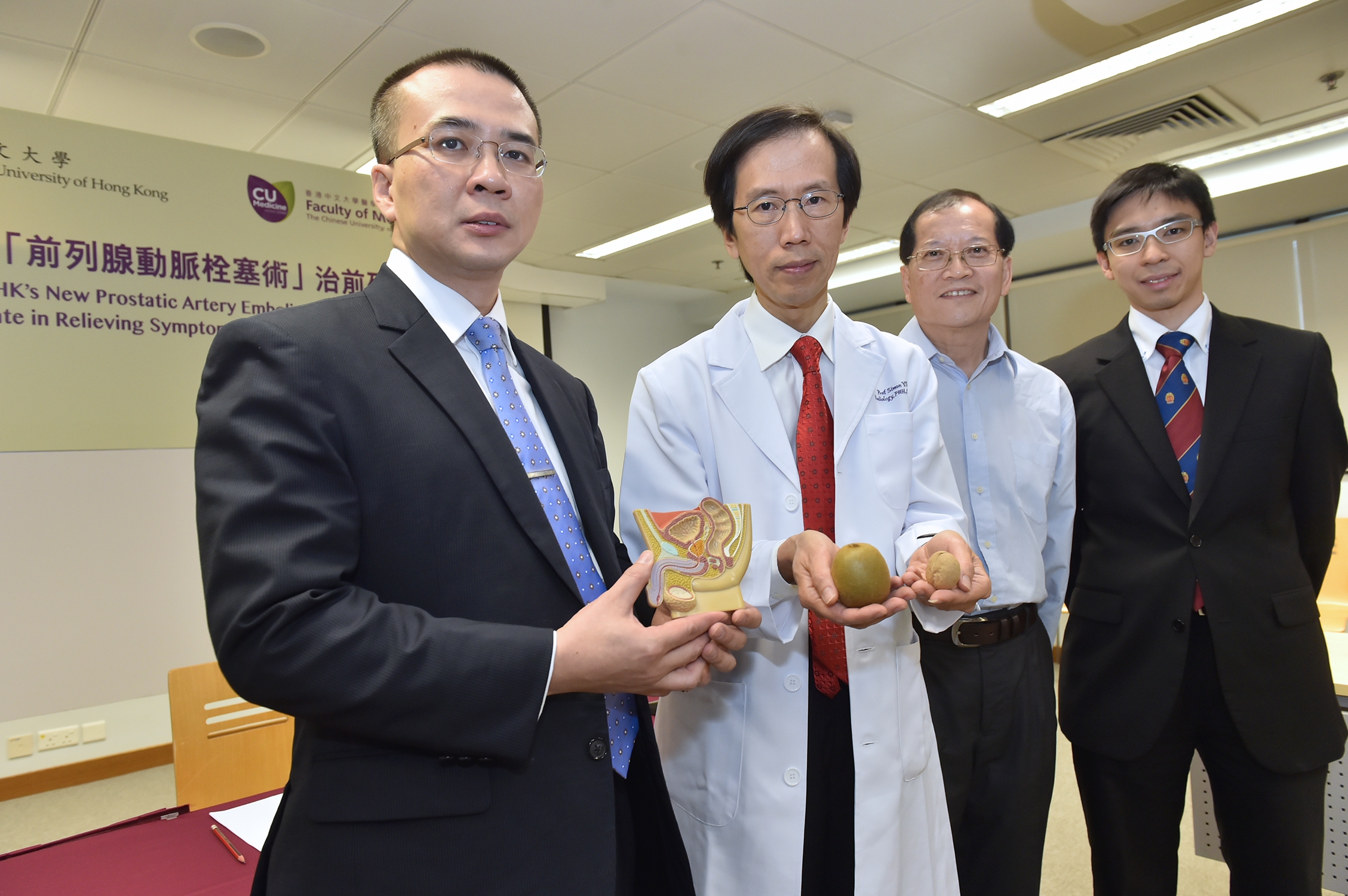
Prof. Simon Chun Ho YU (2nd left), Chairman, Department of Imaging and Interventional Radiology, and Director, Vascular and Interventional Radiology Foundation Clinical Science Center; and his team members in the PAE research, Prof. Anthony Chi Fai NG (1st left), Director of S.H. HO Urology Centre; and Dr. Peter Ka Fung CHIU (1st right), Clinical Assistant Professor (honorary), Division of Urology, Department of Surgery, CUHK.