CUHK
News Centre
CU Medicine proves basophil activation test has much higher diagnostic accuracy for shrimp allergy than conventional allergy tests
Shrimp allergy is the most common food allergy in Hong Kong. In addition to skin reactions and oral symptoms, it can lead to anaphylaxis. The conventional diagnostic approaches include the use of shrimp extracts for skin prick test and measurement of the blood level of shrimp-specific IgE antibody. However, these methods are not accurate, and with many patients have been misdiagnosed as shrimp-allergic. There is thus an unmet need to design a reliable diagnostic method for shrimp allergy. To address this problem, The Chinese University of Hong Kong’s (CUHK) Faculty of Medicine at (CU Medicine) has conducted a study to identify a more accurate test for shrimp allergy diagnosis. The results proved that the basophil activation test (BAT) on individual blood samples showed a sensitivity and specificity of 87% and 94% respectively, which were much superior to those of the conventional methods such as the skin prick test and specific IgE measurement.
The study also proved that tropomyosin, the most important shrimp allergen in the Western population, is not the most appropriate diagnostic biomarker in the Southern Chinese population. Instead, the research team has identified three new shrimp allergens from the giant tiger prawn that are more common and important among patients residing in Southern China. Details of the study have been published in a top international allergy journal called the Journal of Allergy and Clinical Immunology: In Practice.
Shrimp is the most frequent offender causing anaphylaxis in both children and adults
Shellfish is one of the most common food allergies, with shrimp being the most frequent offender causing anaphylaxis in both children and adults. According to a joint study between CUHK and a number of European research institutions, the prevalence of probable shrimp allergy among primary schoolchildren in Hong Kong was 1.05%, whilst for allergies to egg, fish and crab it was 0.2%1. In a territory-wide survey in local nurseries and kindergartens conducted by CU Medicine, 1.28% of pre-school children reported adverse food reactions after shellfish ingestion.2
Dr. Agnes Sze Yin LEUNG, Assistant Professor of the Department of Paediatrics at CU Medicine remarked, “Hives, skin itching and oral symptoms such as itchy mouth are common allergic reactions to shrimp. However, shrimp allergy is also the most common cause of food-induced anaphylaxis requiring emergency admission at local hospitals. As shrimp allergy is a growing health care concern associated with increasing prevalence and low resolution rate in the long term, there is an urgent need to identify objective biomarkers that can accurately diagnose shrimp allergy.”
Study aims to set the stage for accurate alternative diagnostic methods for shrimp allergy
There are several conventional tests for shrimp allergy but every method has its limitation. For example, the skin prick test and specific IgE measurement are known to have insufficient diagnostic accuracy, while “double-blinded, placebo-controlled food challenge”, being the gold standard for shrimp allergy diagnosis, is risky, labour-intensive and expensive. Over the last decade, BAT has been advocated as “food challenge in test tube”. The test is done by analysing the cellular response of a type of white blood cells called basophils in the patient’s blood sample using a flow cytometer.
Professor Ting Fan LEUNG from the Department of Paediatrics of CU Medicine, explained, “Despite its accuracy, the clinical utility of ‘double-blinded, placebo-controlled food challenge’ is limited by cost and safety consideration. Our current study thus aims to set the stage for accurate alternative diagnostic methods for shrimp allergy and reduce the need for oral food challenges.”
BAT is a superior diagnostic test with high sensitivity and specificity
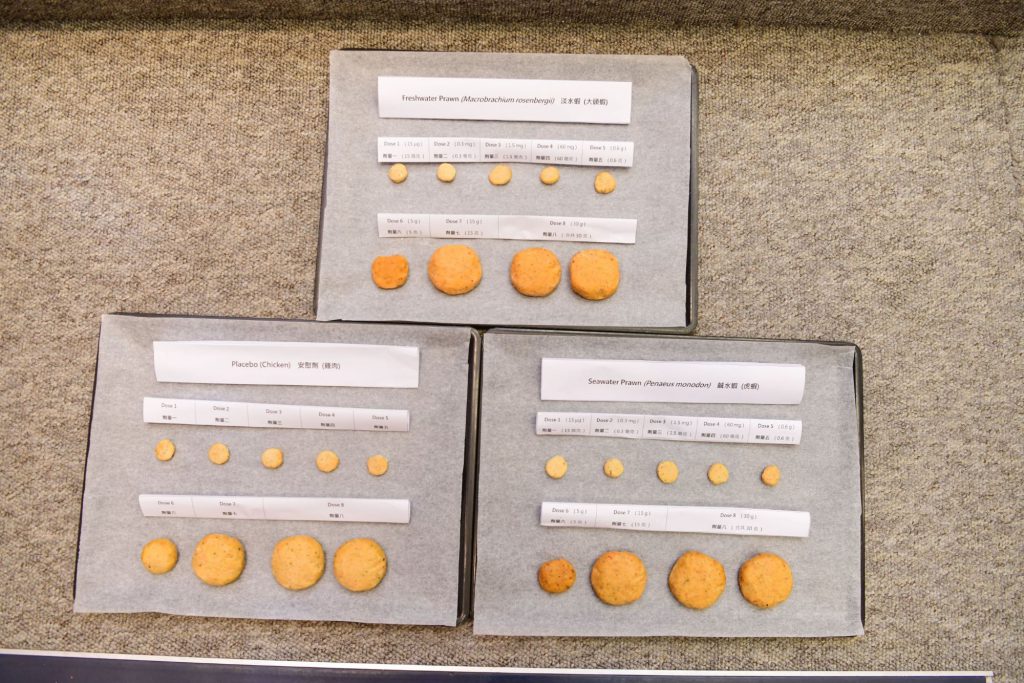
The current study recruited 35 patients who exhibited at least two occasions of immediate allergic reactions after shrimp consumption. All of them underwent “double-blinded, placebo-controlled food challenge”, with 15 of them confirmed to be shrimp-allergic while the remaining 20 participants were tolerant to shrimp.
Both groups of patients underwent the skin prick test, specific IgE measurement and BAT. The results in terms of sensitivity and specificity of each test are shown as follows:
|
|
Sensitivity |
Specificity |
|
Skin prick test |
93% |
28% |
|
Specific IgE measurement |
93% |
35% |
|
BAT |
87% |
94% |
Dr. Christine Yee Yan WAI, Research Associate of the Department of Paediatrics at CU Medicine, said, “Although the sensitivity of the skin prick test and specific IgE measurement is over 90%, the specificity is very low. This indicates their low diagnostic power. By contrast, our results show that BAT is a superior diagnostic test with very high sensitivity and specificity. This demonstrates that performing even a single diagnostic step involving shrimp-BAT can substantially enhance the accuracy for shrimp allergy diagnosis.”
Identified 3 novel shrimp allergens common in Southern China and registered with WHO
The study results also showed that tropomyosin only accounted for 53% of the sensitisation among subjects with challenge-proven shrimp allergy, suggesting that tropomyosin is not the most important shrimp protein causing allergy in Chinese.
In view of this finding, the research team has carried out detailed analyses and identified three new allergens, namely hemocyanin (Pen m 7), triosephosphate isomerase (Pen m 8) and fatty acid-binding protein (Pen m 13), related to shrimp allergy. These shrimp proteins identified from the giant tiger prawn (Penaeus monodon) are common in shrimp-allergic patients in the Southern China. The research team has registered all of them as new shrimp allergens in the Allergen Nomenclature database (http://allergen.org/) of the World Health Organisation and International Union of Immunological Societies, while they have also patented both troponin C (Pen m 6) and fatty acid-binding protein (Pen m 13) as novel diagnostic biomarkers for shrimp allergy.
1 Li J, et al. Comparative Study of Food Allergies in Children from China, India, and Russia: The EuroPrevall-INCO Surveys. J Allergy Clin Immunol Pract. 2020;8(4):1349-1358.e16.
2 Leung TF, et al. Parent-reported Adverse Food Reactions in Hong Kong Chinese Pre-schoolers: Epidemiology, Clinical Spectrum and Risk Factors. Pediatr Allergy Immunol. 2009;20(4):339-346.

CU Medicine proves that the diagnostic accuracy of basophil activation test (BAT) is much superior to that of the conventional methods such as the skin prick test and specific IgE measurement.
From left: Dr. Agnes LEUNG, Assistant Professor; Professor Ting Fan LEUNG; and Dr. Christine WAI, Research Associate, from the Department of Paediatrics at CU Medicine.