CUHK
News Centre
CUHK’s Latest Update on Minimally-Invasive Treatment of Atrial Septal Defect
Congenital heart disease occurs in 1% of newborn infants and 85% of them survive into adulthood due to improved medical care. Atrial septal defect (ASD, also called a hole of the heart) is the commonest defect seen among grown-ups. The heart comprises four separate chambers. The upper chambers, or atria, are divided by a wall called the septum. An ASD is a hole in that septum. When an ASD is present, blood flows abnormally from left to right side chambers. This shunting increases the blood volume burden to the right heart and lung arteries. If left untreated, ASD usually causes complications in adulthood which include heart failure (weakening of right heart muscle), pulmonary hypertension (which is high blood pressure in the lung arteries), cardiac arrhythmias (which are abnormal beating of the heart) and an increased risk of stroke. The common symptoms of ASD include difficulty in breathing during exercise, tiredness or palpitation.
Conventional curative treatment for ASD is surgical repair, which requires general anesthesia and opening of the chest wall, and causes significant morbidity. With the advancement of catheter-based device technology for closure of ASD, most ASD can be closed successfully by a minimally-invasive approach under local anesthesia in the cardiac catheterization laboratory. The septal occluder is attached to a catheter, which is inserted into a vein in the groin and advanced to the heart and through the defect, guided by X-ray and intra-cardiac echocardiography. As the device is slowly pushed out of the catheter, it opens up to cover each edge of the defect, sealing it closed. Over time, tissue grows over the implant and it becomes part of the heart. The obvious benefits of this approach are that it can be performed with local anesthesia and it doesn't create a big surgical scar across the chest the way open-heart surgery does.
Professor Yu Cheuk-man and Professor Lam Yat-yin, Division of Cardiology, Department of Medicine and Therapeutics and the Institute of Vascular Medicine at The Chinese University of Hong Kong (CUHK), in collaboration with other experts at Prince of Wales Hospital(PWH) have initiated a combined service for patients with ASD since 2005. Patients received clinical and echocardiographic examinations at congenital heart disease clinic jointly run by adult and pediatric cardiologists. Case conferences involving adult cardiologists, obstetricians and anesthetists were organized to discuss the best delivery plan for pregnant women with congenital heart diseases. The PWH also introduced the most advanced ultrasound technology, the new generation intra-cardiac echocardiography and real-time 3-dimensional trans-esophageal echocardiography to Hong Kong for the first time, which significantly enhanced patient assessment before treatment as well as procedural safety and success. 75 occluder device-based closure of ASD were performed by cardiologists while only 3 patients needed traditional surgical closure over the past 5 years.
From January 2005 to September 2010, the occluders were successfully implanted in 76 patients (ranged 14-85 years, average age 46 years, 71% female). The primary success rate of the procedure is 98.7% (75 patients). These included 35 patients (47%) with severe pulmonary vascular disease and 21 patients (28%) with large or multiple ASD defects. The mean occluder size implanted was 22±7mm. There was no procedural-related death. The mean procedural time was only 79±37minutes. The average hospital stay was 2 days. At 6-month follow up, 93% (n=70) of patients had decreased in right heart sizes and 91% (n=68) of patients had improvement in symptoms.
In conclusion, implantation of ASD occluder offers a less invasive, safe and effective treatment option for patients suffering from ASD, avoided the need of a major cardiac surgery and prevents the development of ASD-related life-threatening complications.
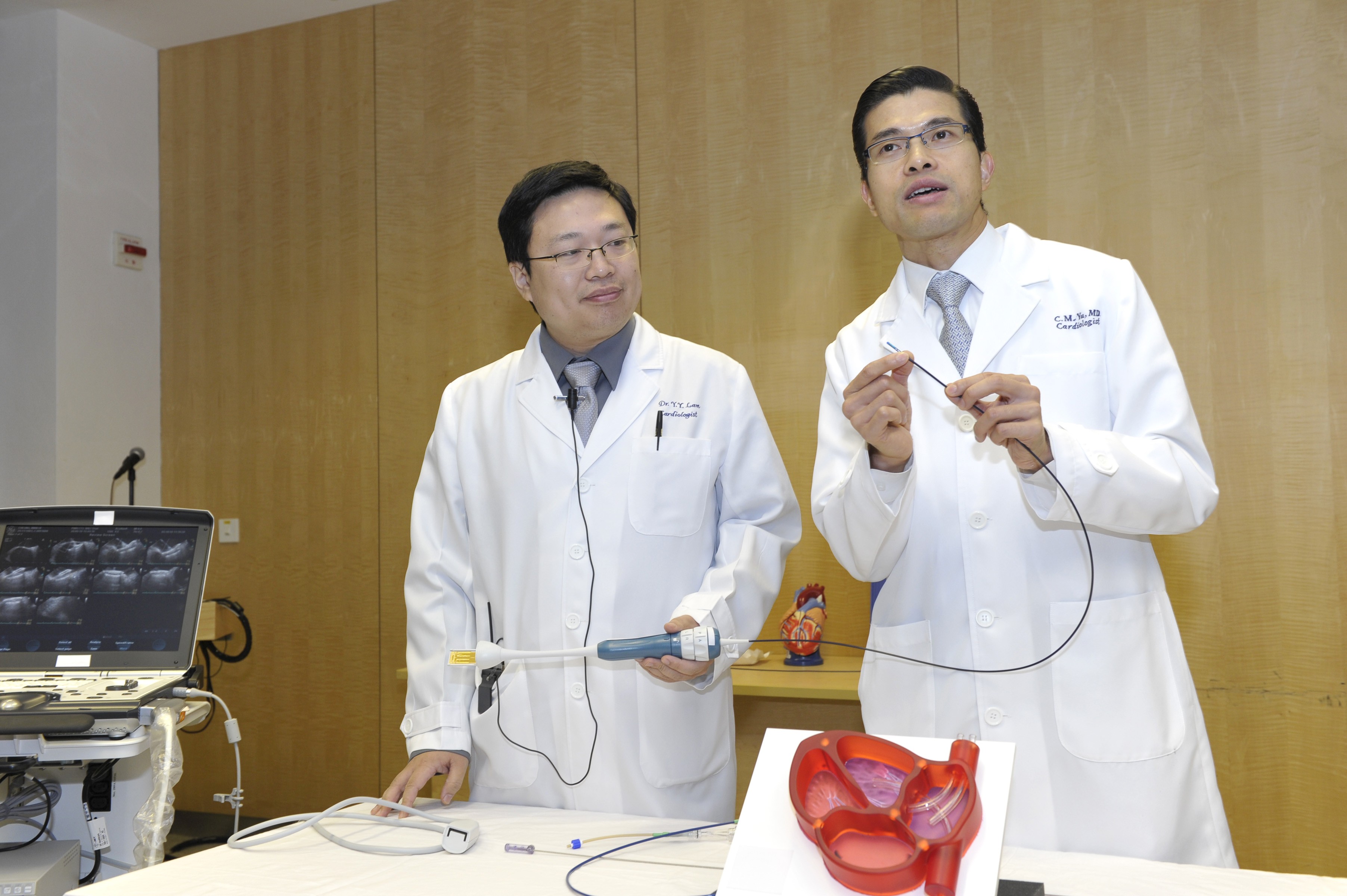
(right) Professor Cheuk Man YU, Chairman, Department of Medicine & Therapeutics and Head of Division of Cardiology, Faculty of Medicine, CUHK and Professor Yat Yin LAM, Associate Professor, Department of Medicine and Therapeutics, CUHK demonstrates how the catheter and occluder were implanted in ASD patients