CUHK
News Centre
CUHK Identifies Outcome Indicators for Benign Prostatic Hyperplasia Patients Receiving Prostatic Artery Embolisation
Benign prostatic hypertrophy (BPH) is a common global health problem among middle-aged and older men which may gradually give rise to very disturbing urinary symptoms. The Faculty of Medicine at The Chinese University of Hong Kong (CU Medicine) has conducted a clinical study on 82 BPH patients receiving Prostatic Artery Embolisation (PAE), a new treatment for BPH. Study results showed that over 80% of the patients had favourable treatment outcomes. For those with post-procedure adverse events related to bladder outlet obstruction, most of them were having intravesical prostatic protrusion with thickness-to-height (T/H) ratio less than or equal to 1.3.
Researchers concluded that the presence of intravesical prostatic protrusion with a T/H ratio less than or equal to 1.3 is an indicator for treatment outcome and occurrence of post-procedure adverse events in BPH patients receiving PAE. The study results have been published in the Journal of Vascular and Interventional Radiology.
Over 80% of the patients receiving Prostatic Artery Embolisation show favourable clinical outcomes
The prostate is a male sex gland which produces a thick fluid that forms part of the semen. BPH is non-malignant enlargement of the prostate gland which may gradually progress to a compression of the urethral canal. This causes an obstruction of the urethra and interferes with the normal flow of urine. Clinical consequences include acute urinary retention, chronic urinary retention and renal failure. According to the Department of Health of the Hong Kong Government, BPH affects more than half of men aged over 60 years, and up to 90% of men aged over 80 years.
BPH patients may be prescribed with medical treatment depending on the size of the prostate gland and the symptoms. If the disease progresses and leads to voiding dysfunction, patients may need to consider surgical treatment. Since 2014, the Department of Imaging and Interventional Radiology at CU Medicine has conducted a clinical study for patients to be treated with PAE, a minimally invasive interventional procedure. It involves embolisation of the prostate using microspheres of 100 to 300 micron in diameter through superselective catheterisation of the prostate arteries under X-ray control. Embolisation leads to ischemic necrosis and volume reduction of the prostate.
The principle investigator of the study, Professor Simon Chun Ho YU, who is the Chairman of the Department of Imaging and Interventional Radiology at CU Medicine, remarked, “82 patients with BPH were treated with PAE from 2015 to 2018 and followed for 3 years. The presence of intravesical prostatic protrusion and its T/H ratio were assessed at baseline using magnetic resonance imaging. Post-procedure adverse events of urinary obstruction within 30 days after PAE were assessed, including acute retention of urine, deterioration in lower urinary tract symptoms, and transient obstruction due to urethral passage of tissue. The long-term clinical outcome of patients after PAE was also observed.”
Study results showed that 69 of the 82 patients (84.1%) had favourable clinical outcomes after PAE. The International Prostate Symptom Score of these patients dropped from 21 at baseline to below 9 after the treatment, indicating that symptoms such as urinary urgency, urinary hesitancy, frequent urination, and weak urine flow were much relieved. These outcomes can last up to 3 years.
Study results facilitate the selection of optimal patients to receive Prostatic Artery Embolisation
For those who had poor clinical outcomes and adverse events after PAE, 12 of the 13 patients had the problem of intravesical prostatic protrusion with a T/H ratio less than or equal to 1.3. These patients needed subsequent medical treatment or even hospital readmission and/or surgery. Therefore, the T/H ratio of intravesical prostatic protrusion can be used before PAE as an outcome indicator for the treatment.
Professor Anthony Chi Fai NG, Director, S.H. HO Urology Centre, Department of Surgery at CU Medicine, remarked, “Compared to transurethral resection of the prostate, which is the usual treatment for BPH, PAE has the obvious advantages of being minimally invasive, with no need for general anesthesia, almost no blood loss, and a minimal risk of sexual dysfunction after the treatment. We knew PAE is a safe and effective treatment. Now we know more about the possible treatment outcomes and the factors affecting it, the identification of a useful outcome indicator for PAE is greatly helpful to doctors in the pre-treatment assessment of patients for PAE.”
Professor YU concluded, “From the results of our study on PAE in the last 6 years, we know that PAE is a treatment with long-term effectiveness, which means patients with BPH have an effective and minimally invasive treatment option. Although PAE could be a risky procedure, our previous study has provided technological improvement in the procedure of PAE. In the current study, we have provided an outcome indicator for PAE which is brand new. We believe it helps to predict the treatment outcome of PAE before it is done and allows doctors to select the most appropriate treatment option for the greatest benefit of patients with BPH. The identification of this outcome indicator is important for the clinical application of PAE, which is well accepted by international experts in PAE, because it is currently the only predictor that precisely indicates which kind of prostate in BPH patients is not suitable for PAE.”
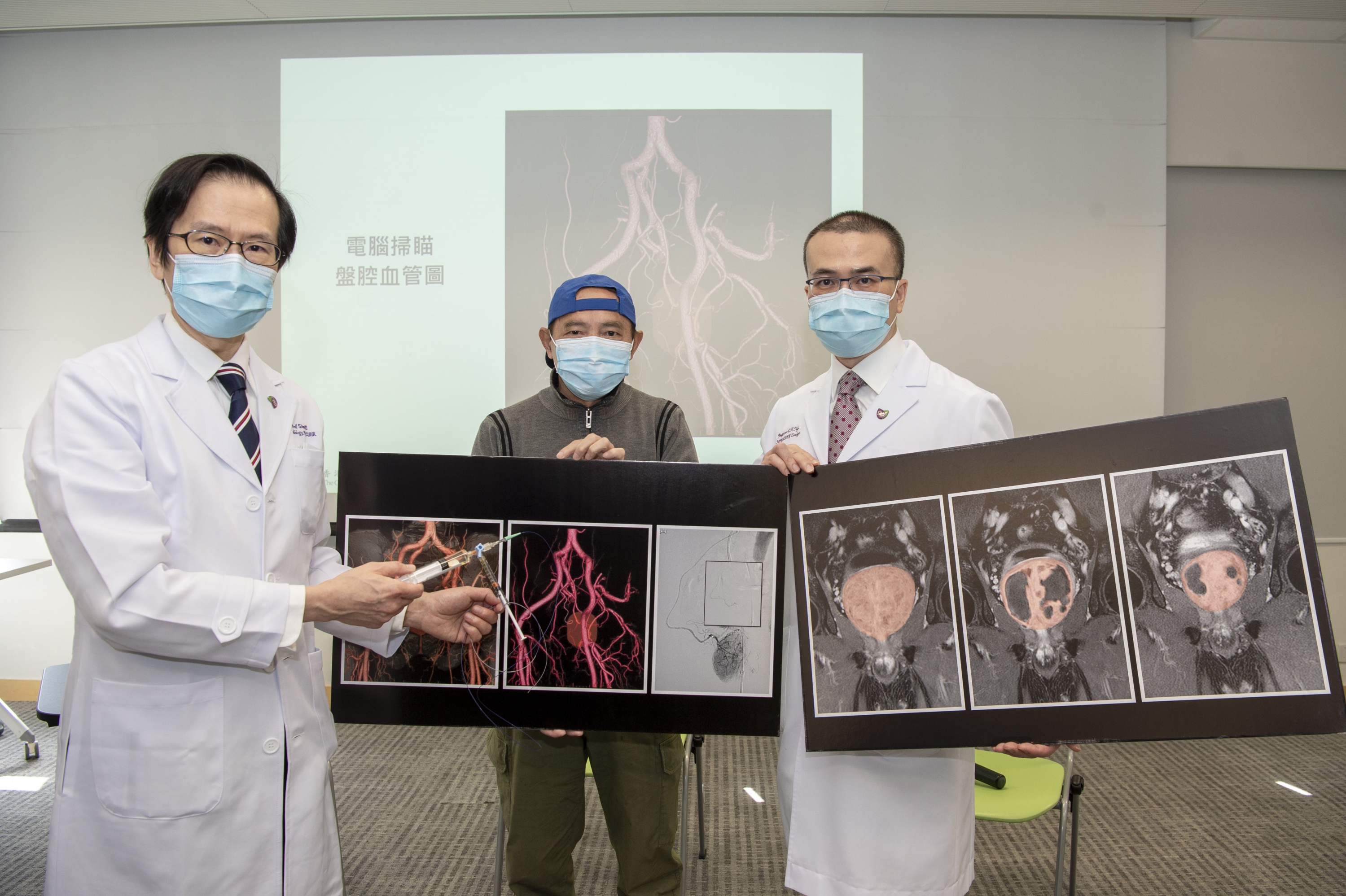
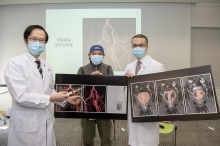
A study conducted by CU Medicine confirms the thickness-to-height (T/H) ratio of intravesical prostatic protrusion can effectively predict the treatment outcome and occurrence of post-procedure adverse events in BPH patients receiving PAE. (From left) Professor Simon YU, Chairman of the Department of Imaging and Interventional Radiology; BPH patient Mr. Tam; and Professor Anthony NG, Director of the S.H. HO Urology Centre of the Department of Surgery, CU Medicine.
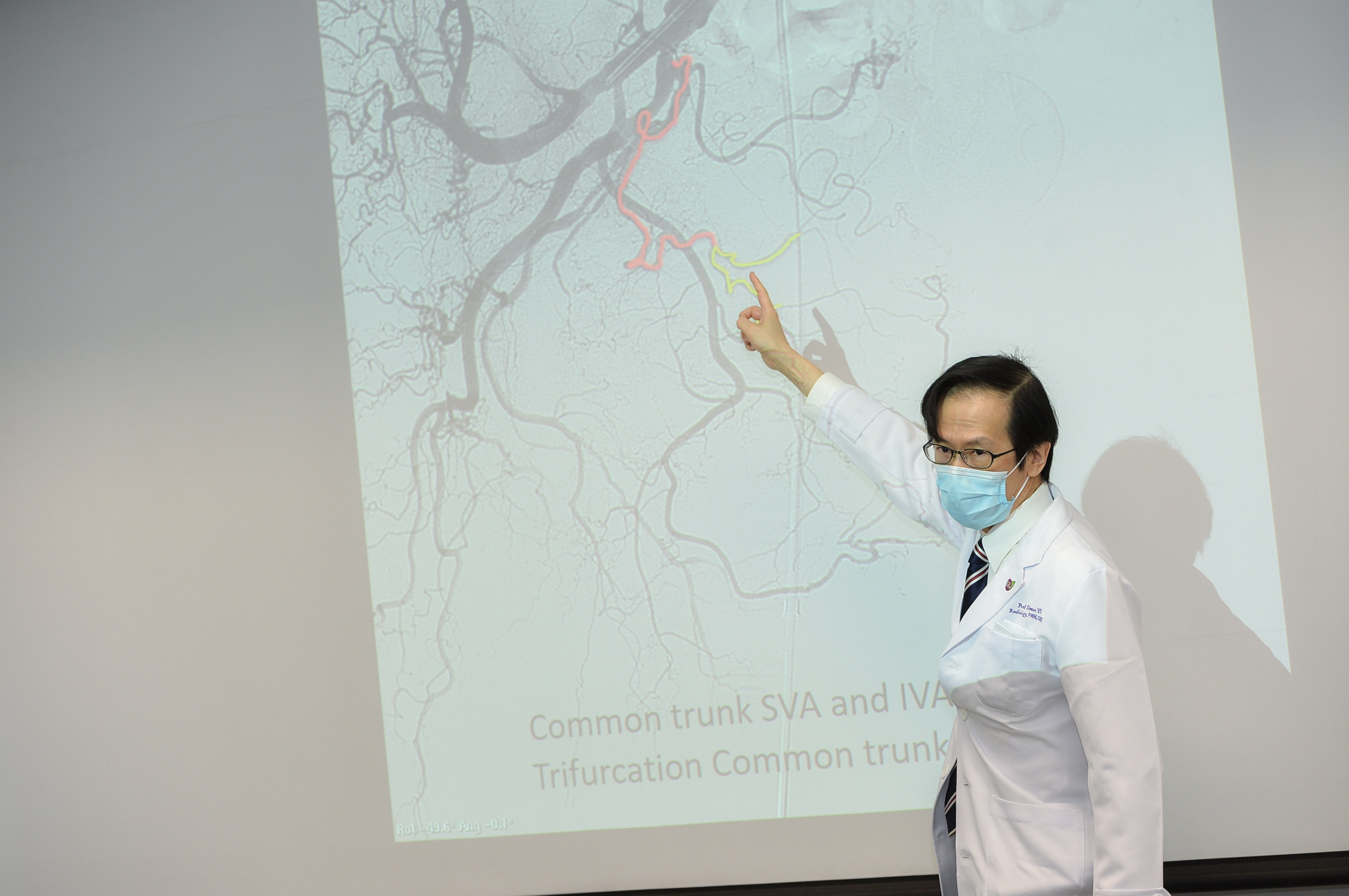
Professor Simon Yu states that results of the current study help to predict the treatment outcome of PAE before it is done and allow doctors to select the most appropriate treatment option for the greatest benefit of patients with BPH.
Compared to transurethral resection of the prostate, which is the usual treatment for BPH, Professor Anthony Ng says that PAE has the obvious advantages of being minimally invasive, with no need for general anesthesia and almost no blood loss.