CUHK
News Centre
CUHK Successfully Conducts Asia-Pacific’s First Hybrid Operating Room Non-invasive Bronchoscopic Microwave Ablation to Treat Lung Cancer
Thoracic surgical professors from the Faculty of Medicine of The Chinese University of Hong Kong (CUHK) successfully performed Asia-Pacific’s first non-invasive Bronchoscopic Microwave Ablation (BMA) in hybrid operating room for lung cancer treatment on 4th March 2019. The world renowned team in hybrid operating room thoracic procedures and electromagnetic navigation bronchoscopy has combined these technologies to allow high precision delivery of a BMA probe into the lung cancer, directly destroying the lesion. This novel approach to lung cancer treatment is totally scarless and has minimal morbidity compared with lung cancer surgery. As of now, the thoracic team has helped three patients with lung cancer by this technique. All were successful and discharged home one to two days after the procedure, without complications.
BMA – A new treatment option for lung cancer patients
Lung cancer remains one of the most common and deadliest cancers in Hong Kong. The best outcomes are achieved when patients are diagnosed and treated in the early stage. In the past, the standard of treatment was to conduct surgery for early stage lung cancers, and chemotherapy with or without radiotherapy for more advanced stage diseases. A new treatment option using BMA in select groups of lung cancer patients can avoid the trauma, pain, scars and complications associated with surgery.
Cancer cells are effectively destroyed by microwave energy emitted from the ablation catheter
Through the use of electromagnetic navigation bronchoscopy, surgeons can deploy the catheter tip for ablation into the lung cancer, and destroy the diseased tissue by the emitted microwave energy. Dr. Rainbow Wing Hung LAU, Clinical Assistant Professor (honorary), Division of Cardiothoracic Surgery, Department of Surgery, Faculty of Medicine, CUHK, explained, “Microwave energy emitted from the catheter tip excites water molecules within the treatment zone of the lung tissue, raising the surrounding temperature to above 60°C. At above 60°C, all living cells, including cancer cells will die, effectively destroying the cancer.”
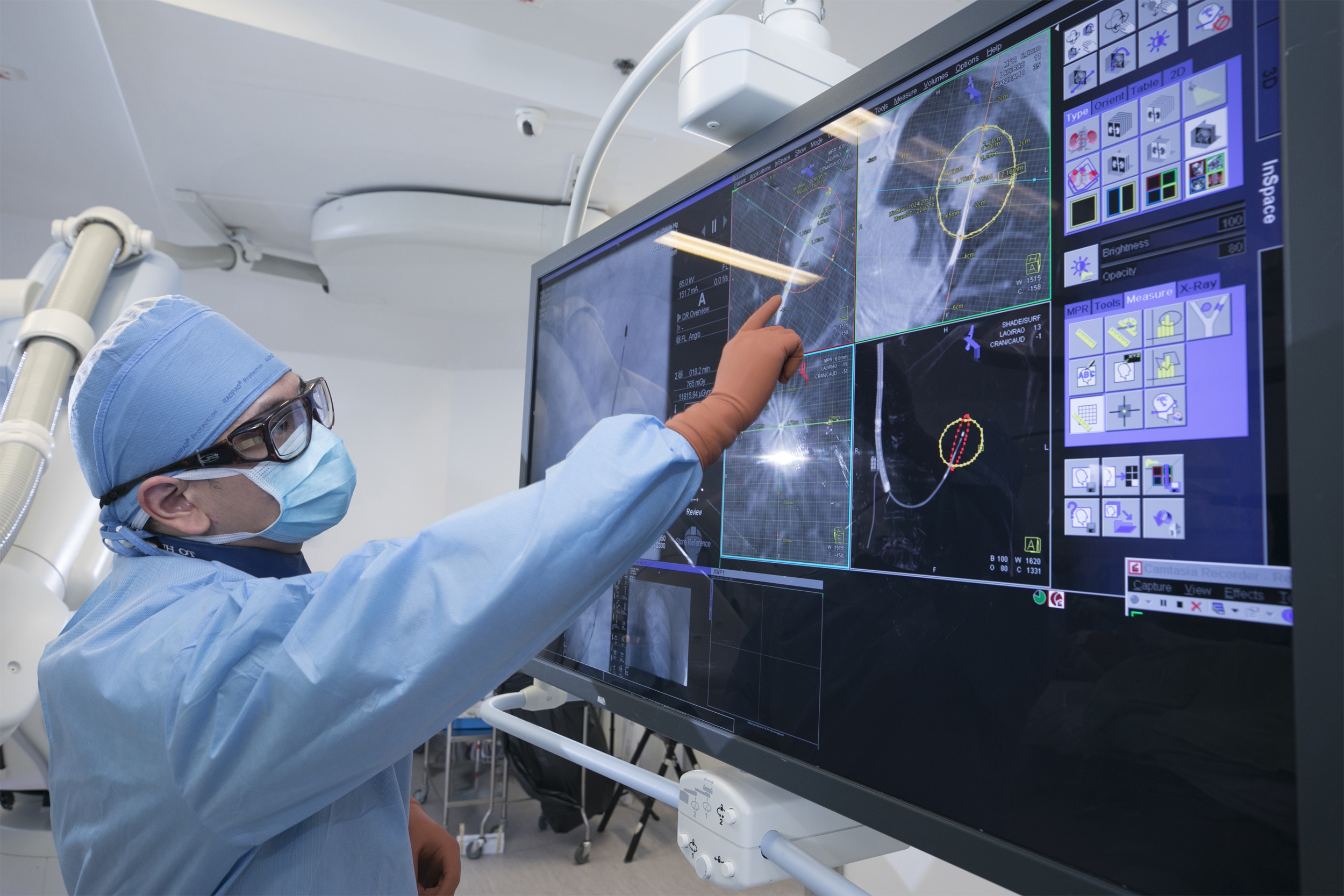
The whole procedure is performed under a light general anaesthesia in the hybrid operating room under the guidance of the real-time 360-degree cone-beam computed tomography scans to ensure proper placement of the microwave catheter, and the ablation is successful in destroying the cancer. The actual lung cancer ablation takes only 10 to 20 minutes to complete, and the BMA catheter is then removed. The patient is woken up and chest x-ray is done to ensure there are no complications before discharging the patient home.
Patients of advanced age, with limited lung function or with lung metastases can be recommended for BMA
BMA can be recommended to:
– Patients with primary lung cancer who are not suitable for surgery because of advanced age, major co-morbidities or with limited lung function; or those who decline surgery for personal reasons
– Patients with small ground glass opacities that can be pre-cancerous or very early lung cancers
– Patients with lung metastases
– Patients with lung cancer who have had previous radiotherapy to the same region of the lung
– Patients with multiple or bilateral lung cancers requiring local control
As in all medical procedures, it is important to select the appropriate patients. The best outcomes are achieved when:
– Lung cancer to be ablated is less than 3 cm. This is because the maximum treatment zone of the microwave catheter is 4.2 cm
– Lung cancer is at the outer two-thirds of the lung
– Lung cancer is away from pulmonary blood vessels
BMA is non-invasive and without blood loss, thus the hospital stay is significantly shortened
Surgery is associated with access trauma, blood loss, pain (which can be chronic), and scars. Complications from surgery can occur that lengthen the hospital stay and lead to a prolonged period of recovery, or even permanent disability. Even with the most modern and advanced minimally invasive surgical approaches, surgical morbidity and complications are less but are inevitable.
Dr. Calvin Sze Hang NG, Associate Professor, Division of Cardiothoracic Surgery, Department of Surgery, Faculty of Medicine, CUHK explained, “The BMA approach when compared with lung surgery has reduced blood loss (no blood loss in most cases), is painless in most patients, has a shorter hospital stay, minimal effect on lung function, and is totally non-invasive with no wounds. Furthermore, the procedure could have lower risk of complications; for example, lower risk of pneumonia, pleural infection and prolonged airleak.”
There are other advantages. Bronchoscopic ablation can be repeatedly applied to the lung, or to previously ablated areas. Though in overseas experience, pleural effusion and pneumothorax may occur in a small number of patients, for most no intervention is required.
More efficient and accurate deployment of the BMA catheter by robotic bronchoscopy
Dr. Ng stated, “The development of robotic bronchoscopy may allow more efficient and accurate deployment of the BMA catheter into the lung cancer, potentially shortening the operation time and also further reducing complications.”
Dr. Ng added that in patients with more advanced lung cancers who are receiving chemotherapy and radiotherapy, there may be an additional role for bronchoscopic ablation in achieving good local control of the cancer. Future studies by CUHK will determine the potential benefits of BMA in these clinical cases.
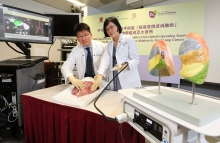
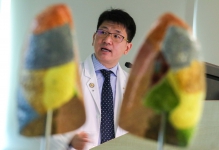
Thoracic surgical professors from the Faculty of Medicine of CUHK successfully performed Asia-Pacific’s first non-invasive Bronchoscopic Microwave Ablation (BMA) in hybrid operating room for lung cancer treatment. Featured in the photo are Dr. Calvin NG (left), Associate Professor, Division of Cardiothoracic Surgery, Department of Surgery, Faculty of Medicine, CUHK; and Dr. Rainbow LAU, Clinical Assistant Professor (honorary) from the same division, simulating the process of the treatment.
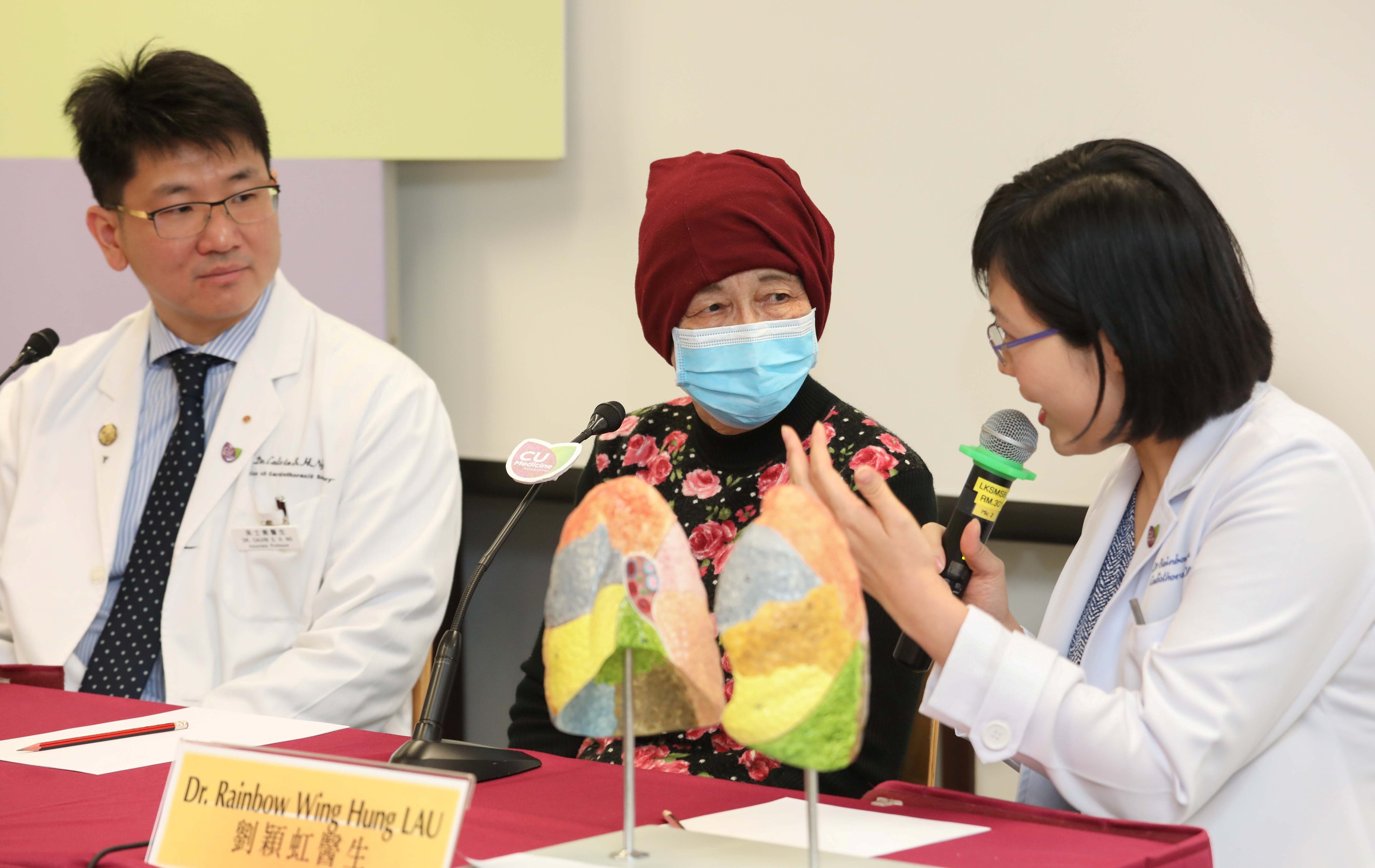
Dr. Calvin NG explains that the BMA approach can reduce blood loss (no blood loss in most cases), is painless in most patients, allows a shorter hospital stay, has minimal impact on lung function, and is totally non-invasive without incision. Furthermore, the procedure could have lower risk of complications.
Dr. Rainbow LAU explains that microwave energy emitted from the catheter tip excites water molecules within the treatment zone of the lung tissue, raising the surrounding temperature to above 60°C and effectively destroying the cancer.
(Middle) Ms. Chan (pseudonym), a patient who had received BMA for the treatment of lung cancer, says that she was able to go out for lunch with her family three days after the treatment. No complications have been observed so far.
The actual scene showing BMA of lung tumours in the hybrid operating room. Featured is the surgeon precisely deploying microwave ablation catheter into the lung tumour with the assistance of cone beam computed tomography (CT) in the hybrid operating room.
The actual scene showing BMA of lung tumours in the hybrid operating room. The photos show the confirmation of adequate ablation of cancer cells through advanced evaluation of CT images.