CUHK
News Centre
CU Medicine Found SARS-CoV2 in Infants’ Stool A Coronavirus Testing Centre Is Established for Paediatric Population to Identify Silent Carriers
Researchers from the Faculty of Medicine of The Chinese University of Hong Kong (CU Medicine) found for the first time that COVID-19 patients have active and prolonged gut viral infection, even in the absence of gastrointestinal (GI) symptoms. After respiratory clearance of coronavirus, the activity of viral infection and replication will still persist in the gut. The study result has impacted the clinical management of COVID-19 patients and was published in the international medical journal GUT.
Considering that stool tests are safe, accurate and non-invasive, CU Medicine offered free stool test to airport arrivals from 29 March. As of 31 August, more than 2,000 stool samples have been tested and 6 children were confirmed with COVID-19 infection, and the detection rate is 0.28%. Starting from today (7 September), CU Medicine will provide up to 2,000 COVID-19 tests per day. This will include stool screening test provided to specific groups targeted by the Department of Health. It is hoped that this helps identify asymptomatic people carrying the COVID-19 virus as early as possible in order to stop its spread in our community.
Active and Prolonged GI Infection Even in the Absence of GI Symptoms and After Recovery
To better understand the activity and infectivity of COVID-19 virus in the GI tract during the disease’s course, researchers from CU Medicine investigated the stool samples of 15 COVID-19 patients in Hong Kong between February and April 2020. The study provides evidence that there was active gut viral infection in 7 patients even in the absence of GI symptoms. Three patients continued to display active viral infection up to 6 days after clearance of the virus from their respiratory samples.
At the same time, it is noted that gut microbiota of patients with high SARS-CoV-2 infectivity was characterised by enrichment of pathogens and loss of “good” bacteria that are capable of producing short-chain fatty acid.
Professor Siew Chien NG, Associate Director of the Centre for Gut Microbiota Research at CUHK, explained, “Active and prolonged viral activity in the gut of COVID-19 patients, even in the absence of GI manifestations and after recovery, highlights the importance of long-term coronavirus and health surveillance and the threat of potential faecal-oral viral transmissions. Therapeutics approaches including limiting gut viral activity and modulating gut microbiome composition and functionality should be explored.”
Successfully Identified Six COVID-19 Patients through Stool Screening Test
CU Medicine’s earlier studies found that the COVID-19 virus was detectable in the stool samples of all patients, regardless of the degree of illness. Starting from March 29, CU Medicine has offered to conduct, for free, stool tests for asymptomatic children or the needy coming to Hong Kong by air to screen for possible COVID-19. The Department of Microbiology of CU Medicine processes the stool specimens in its laboratory and provides the results to the Government the next day when the stool specimens are received. As of 31 August, 2,128 stool tests have been conducted and 6 children were confirmed to have COVID-19 infection through the stool screening test conducted by CU Medicine, and the detection rate is 0.28%.
Last month a 9-month-old baby girl in Macau mistakenly swallowed a broken sampling rod when her throat swab was being collected for virus test. Professor Paul Kay Sheung CHAN, Chairman of the Department of Microbiology and Associate Director of the Centre for Gut Microbiota Research, who is in-charge of the testing service of CU Medicine, highlighted, “The viral load in the stool of infant and children is many times higher than that in adults, and could be equivalent to that of adult respiratory samples. The activity of viral infection and replication also persist longer in the guts of infant and children. Stool specimens are more convenient, safe and non-invasive to collect in the paediatric population and can give accurate results. This makes stool test a better option for COVID-19 screening in babies, young children and those whose respiratory samples are difficult to collect.”
Providing Up to 2,000 COVID-19 Tests Per Day and Focus on the Groups that Need Stool Test
To enhance Hong Kong’s capacity to test for COVID-19, CU Medicine has received government support to increase laboratory manpower and equipment for testing. Starting from today (7 September), CU Medicine can provide up to 2,000 COVID-19 tests per day. In addition to specimens of respiratory tract, CU Medicine will continue to work with the Department of Health to focus on providing stool tests to local high-risk babies and young children, the paediatric population returning to Hong Kong from high risk areas, and those people who have difficulties in collecting specimens of sputum, nasal and throat swabs.
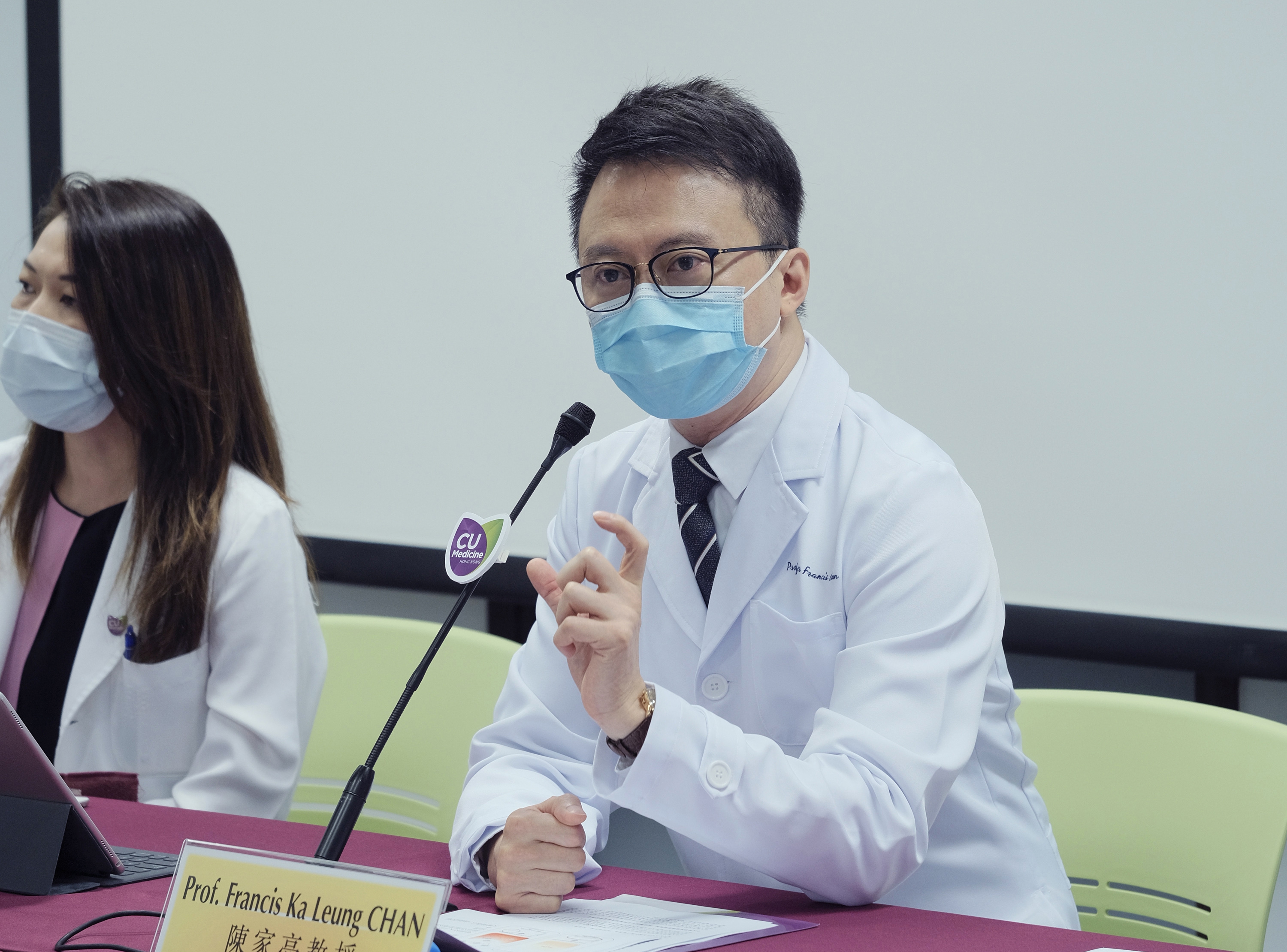
Professor Francis KL CHAN, Dean of the Faculty of Medicine and Director of the Centre for Gut Microbiota Research at CUHK remarked, “Among the confirmed cases in the territory, we note that there is more than one COVID-19 patient who had stool test positive while tests for respiratory samples were negative. Stool test is accurate and safe, making it suitable and more effective for COVID-19 screening for specific groups of people. Some countries including the U.S. Food and Drug Administration, are currently in contact with us for details and arrangements of stool tests for COVID-19.”
CUHK established a Coronavirus Testing Centre for paediatric population to identify silent carriers of COVID-19 viruses, with a target to provide up to 2,000 COVID-19 tests per day. (From left) Professor Paul CHAN, Chairman of the Department of Microbiology and Associate Director of the Centre for Gut Microbiota Research; Professor Francis CHAN, Dean of CU Medicine and Director of the Centre for Gut Microbiota Research; and Professor Siew NG, Associate Director of the Centre for Gut Microbiota Research, at CUHK.
Professor Francis CHAN states that some countries including the U.S. Food and Drug Administration are currently in contact with CU Medicine for details and arrangements of stool tests for COVID-19.
Professor Siew NG highlights that the activity of viral infection and replication will still persist in the gut of COVID-19 patients even after respiratory clearance of coronavirus. The study result has impacted the clinical management of COVID-19 patients.
Professor Paul CHAN states that stool specimens are more convenient, safe and non-invasive to collect in the paediatric population and can give accurate results. This makes stool test a better option for COVID-19 screening in babies, young children and those whose respiratory samples are difficult to collect.